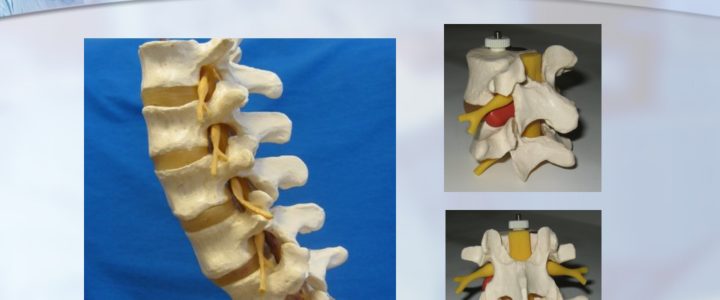
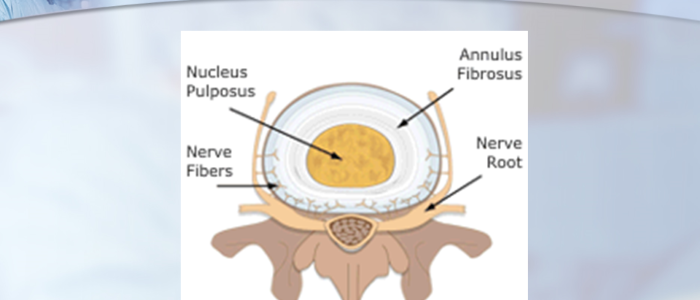
Since 2000, Dr. Luis Lombardi has served as a privately practicing non-traumatic spine surgeon in Los Angeles, California. Dr. Luis Lombardi draws on a comprehensive knowledge of both normal and abnormal vertebral anatomy. The human spine is made up of 33 interlocking vertebrae, 24 of which are independently mobile. Each of these vertebrae consists of a cylindrical solid structure known as the vertebral body, which can withstand body weight and bears compression generated from pressure and movement. On the interior side of this structure lies the vertebral arch, which together with the vertebral body makes a circle around the spinal canal. The vertebral arch connects to a series of bony processes, to which the skeletal muscles connect. In between each pair of vertebrae lies the intervertebral disc. The disc consists of a shock-absorbing nucleus, which is contained within a harder protective annulus. The exterior third of the annulus contains pain-sensitive nerve fibers that activate in instances of disc damage. The primary nerves in the spine, however, pass down the spine behind the vertebrae and discs. Located close to the interior edge of the disc, the nerves branch out to become nerve roots, which come together to become the larger nerves of the legs
Anatomy of the Vertebra and Disc by Dr. Luis Lombardi